Coronavirus disease (COVID-19) testing is probably something you’ve heard a lot about. Contact your health care physician or your local health departmentExternal Link Disclaimer very away if you suspect you have COVID-19 and require a test. You may also look for a community testing location in your area or purchase an FDA-approved at-home test. Some FDA-approved at-home testing can provide findings in minutes. Others will ask you to send the sample to a lab for testing.
If you have a current COVID-19 infection, diagnostic testing can reveal if you need to quarantine or isolate yourself from others. Diagnostic techniques such as molecular and antigen testing can determine whether or not you have a current COVID-19 infection. A nose or throat swab, or saliva collected by spitting into a tube, is used to collect samples for diagnostic testing.
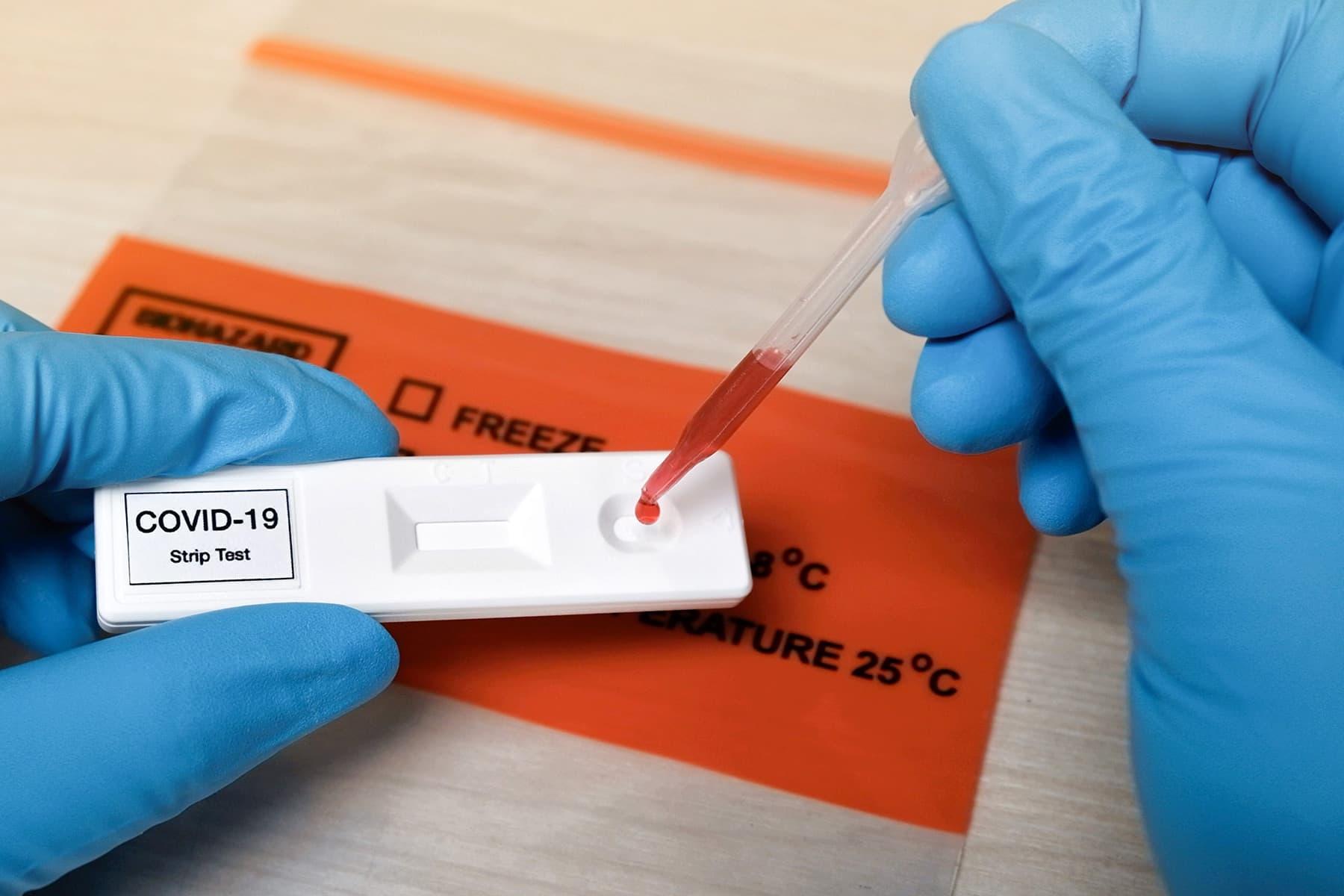
Antibody testing seek for antibodies produced by your immune system in response to the virus that causes COVID-19, SARS-CoV-2. Antibody testing should not be utilized to diagnose a COVID-19 infection that is still ongoing. Antibodies can take days or weeks to form after an illness, and they can linger in your blood for weeks or months after you’ve recovered. Blood from a fingerstick or blood taken by your doctor or other medical professionals are commonly used for antibody testing.
Different Types of COVID Tests
Here is the latest list of all types of COVID tests that you should know about.
1. Molecular Test (Aka RNA or PCR Test)
These tests are the most sensitive for identifying a current infection, and the results are quite reliable. If you or your doctor suspect you have COVID, you may want to take one. If you need to show to your employer or institution that you are not currently infected before returning to work or campus, you may be requested to take this sort of test.
In most situations, a health care professional will use a specialized swab to collect mucus from your nose or throat. (Certain molecular tests now utilize saliva, which may be more pleasant for some people.) According to the US Food and Drug Administration, PCR tests are short for polymerase chain reaction, which is the lab technique used to detect the virus’s genetic material (FDA). According to the Mayo Clinic, depending on whether the sample is tested onsite or transferred to an outside lab, turnaround time can range from minutes to days or longer.
The gold standard for testing is still a nasopharyngeal swab, which penetrates deep into your nose and to the back of your throat. However, at-home test kits have recently been available, allowing consumers to collect their own sample (mucus or spit) and send it to a lab for examination overnight. These test kits are simple to use and may be less frightening than long-swab testing utilized in hospitals. Furthermore, one tiny research shows that when consumers are given the correct method for obtaining their own samples, self-testing can produce findings as accurate as those obtained by healthcare professionals.
2. Antigen Test (Aka Rapid Test)
Because the turnaround time is significantly faster than an RNA test, this sort of diagnostic test is sometimes referred to as a “rapid test.” It’s also less expensive to make. As a result, antigen testing are increasingly being used to screen large groups of people, such as at airports, according to a new research in the journal Nature.
Antigen testing is similar to molecular testing in terms of how it works for patients. To gather a sample for testing, your health care practitioner will swab the back of your nose or throat. On the other hand, an antigen test can give a response in an hour or less, rather than days, according to the FDA. Antigen testing are quite accurate, so if you test positive, you’re probably right. The concern is that these tests have a higher chance of missing current infection. If you have COVID symptoms but your blood test comes back negative, your doctor may request a molecular test to rule out a false negative.
Some antigen tests may be done immediately in your doctor’s office, so you won’t have to go to a lab. These “point-of-care” diagnostics are mainly utilized in emergency rooms, doctor’s offices, and outpatient clinics. (Note: Antigen testing are not all quick point-of-care tests.) In September, Roche’s fast PCR-based combo test for SARS-CoV-2 and the flu was approved emergency use by the FDA.)
3. Antibody Test (Aka Serology Test or Blood Test)
This test searches for coronavirus antibodies. Antibodies are proteins produced by your immune system to combat external invaders such as viruses. Active coronavirus infection cannot be diagnosed with a COVID-19 antibody test. It just informs you whether or not you’ve been infected in the past, even if it was months ago. Antibodies aren’t detected for at least a few days after an infection has begun.
The FDA does not approve At-home antibody testing. You’ll need to see a doctor, who will draw blood from a vein in your arm or collect a blood sample from a finger prick. The great majority of these tests are completed in a central lab, which can take several days to complete. However, the FDA recently authorized the first antibody point-of-care coronavirus test, allowing doctors’ offices, hospitals, urgent care centres, and emergency rooms to receive a result in as little as 15 minutes using blood from a patient’s fingertip.
According to the Mayo Clinic, antibody testing should be done at least 14 days following the onset of symptoms. It’s possible that if you test too soon, when your immune system is still putting up a fight, the result won’t be accurate. When someone seeks medical help late in the course of their disease, antibody testing is sometimes combined with viral testing. It may also aid in the confirmation of a diagnosis of COVID-related Multisystem Inflammatory Syndrome in Children. Is it true that having antibodies to SAR-CoV-2 means you’re immune to subsequent COVID infections? Researchers are still unsure, but new research suggests that previous episodes may give some protection.
According to the FDA, antibody testing can offer information on the prevalence of the illness in the population as well as the frequency of asymptomatic infection in the present pandemic. As of the time of publication, the information in this report is correct. However, because the situation around COVID-19 is still developing, some statistics may have altered after publication. While Health makes every effort to keep our stories up to date, we also advise readers to use the CDC, WHO, and their local public health agency as resources to remain updated on news and recommendations for their own areas.
4. Rapid Blood Test
The assays we employ at our facilities are fast blood tests that evaluate immunoglobulin levels in order to determine the cluster of various antibodies. Antibodies are produced by our immune system, which is in charge of defending us against illnesses. Antibodies protect us from pathogens such as bacteria, allergens, and viruses. Antibodies change depending on the type of infection they are combating. The quick blood tests allow us to assess the clusters of these distinct types of immunoglobulins and determine if they are protected against the SARS COVID-19 by antibody formation. As the illness develops, antibody levels begin to rise.
When an antibody is generated in reaction to a specific substance, the immune system recognizes it the next time it enters the body and “remembers” the defence response, generating the same antibodies as before. The fast assays we’ve developed look at IgG and IgM levels to see if active immunoglobulin (IgM) is present as a response to an infection (COVID-19) (an acute infection). Or if there is a “memory,” immunoglobulin (IgG) formed against COVID-19, implying that you experienced the illness and that your immune system now has a protective reaction. Our rapid tests have been approved by the Federal Commission for the Protection Against Sanitary Risks (COFEPRIS), as published in the official federation newspaper on May 18th, 2020.
5. Rapid Antigen Test
The World Health Organization just authorized the fast antigen test. It’s a brand-new COVID-19 diagnostic test. This test looks for antigens, which are proteins found in the virus’s protective coating. Once the SARS CoV-2 virus is discovered, it is assumed that the patient has caught the virus and will develop COVID-19 illness and spread the infection.
The antigen test is popular because it is quick to do, taking only 20 to 30 minutes from the time the sample is collected. We utilize a totally sealed kit for this test, which includes a lengthy swab for taking a sample from the nasopharynx. The material is then processed to identify the protein chains and determine the presence of the SARS CoV-2 virus. The outcome is either “Positive” or “Negative.” Within the first seven days of suspected COVID-19 symptoms, the fast antigen test performs better. The chances of giving a false negative rise beyond this time frame.
6. Pcr Test (Polymerase Chain Reaction)
The PCR (Polymerase Chain Reaction) test is the most common method for detecting the SARS-CoV-2 virus, which causes COVID-19 in humans. The PCR test is a molecular biology lab test that looks for genetic material from disease-causing microorganisms. This material is maximized by collecting a tiny sample of organic material and using it to identify a specific genetic chain of the agent. A version of the RT-PCR (Reverse Transcription Polymerase Chain Reaction) is used to test for SARS-CoV-2. In this test, we look at the pathogen’s RNA rather than its DNA. A “Reverse transcriptase” analyses the RNA and converts it into complementary DNA.
It is then maximized for identification after this is completed. The sample is obtained by spinning a long cotton swab between both nostrils and the throat to get a nasopharyngeal exudate. The PCR test is extremely specific and effective in distinguishing the virus from other diseases, and it is also highly sensitive, even when the pathogen is present in small amounts or during the early stages of infection.
7. The Future Of Testing
Infectiousness: Neither antigen nor molecular testing can determine whether or not a person has an infectious virus, which means the virus is not only present but also capable of invading cells and replicating, resulting in an infection. This is something that can be measured, but just a few laboratories in the United States are doing it. One of them works at the Bloomberg School of Public Health at Johns Hopkins University. These tests need highly specialized labs since they entail producing the virus, and they are not available to the general public.
In the lack of extensive infectivity testing, our best guess for whether a person may transmit the virus is based on time: most individuals will stop harbouring infectious virus after around 12 days of symptoms. Furthermore, you may be infected with the virus for two or three days before symptoms appear.
Testing in New Ways: Because nasal and throat swabs are uncomfortable”especially for individuals who need to be tested frequently”researchers are looking at less intrusive approaches including breath-based tests and improving saliva tests.
Pooled Testing: Using super-sensitive PCR testing, a group of specimens may be “batched” and examined collectively rather than individually to see if anyone in the group is infected. Individuals can be examined if the pooled test is positive. This approach, which has already been used in low-resource situations, is gaining popularity as a means to get more mileage out of limited testing materials by eliminating the need to test a large number of people individually. It works best in places where the virus is uncommon.
Frequently Asked Questions (FAQs)
What Is The Difference Between The IGM And IGG Fast Tests?
IGM antibodies are created in our bodies when an external microorganism attacks us, and our immune system employs them to counteract the harmful impact of that microbe, which is why they emerge during the active disease’s second stage.
What Is The Purpose Of The IGG Test?
The IGG allows us to determine whether or not we have been exposed to the illness. We are no longer infectious if we have had contact with the disease since we have already produced antibodies to the virus. This test simply determines whether or not we have the illness, not if it is active.
What Does It Imply If Both The IGM And The IGG Tests Are Positive?
This indicates that it is most likely between the tenth and fourteenth day of the illness. IGM antibodies might last for up to 25 days after they first emerge. IGG antibodies start to develop around day 10, although they can last for up to three months.
What Does It Indicate If IGM Is High But IGG Is Low?
During this stage of the illness, the body launches the most aggressive fight against the virus via IGM antibodies. This indicates that you are at an infectious stage of the sickness and should self-isolate as directed by your doctor.
What Does IGG Positive Signify If IGM Is Negative?
The illness is still present, but it is no longer infectious. And is less likely to contract COVID-19 in the future.
When May The COVID-19 Virus Be Detected With A PCR Test?
At least 24 to 48 hours following interaction during the first phase (before to the development of symptoms). (-7) should be written as -7 instead of 24 to 48 hours. The virus might spread to other organs of the body after 7 days.
What Exactly Does a PCR Test Entail?
This test is carried out using a swab placed via the nose until it reaches the back of the throat, where it is rotated to acquire a sample of mucus or nasal discharge, as this is where the virus is most concentrated during the -7 and first 7 days.
What Is The Purpose Of This Test?
DNA, or deoxyribonucleic acid, is the subject of this test. In their DNA, each individual or thing contains features that are unique to them (genetic identity) The assay extracts DNA from the virus in order to detect the COVID-19 portion of DNA.
Is This The Most Useful Test?
Yes, diagnosing COVID-19 in the early stages (days) when symptoms have not yet emerged is the most beneficial. (It’s been a week since the exposure)
When Should I Schedule This Test?
If you suspect you’ve been infected or had in touch with someone who has tested positive for COVID-19, we recommend doing this test.
What’s The Difference Between PCR and an Antibody Test?
If you have the infection within the first (-7 days) days, PCR can tell you if you have it. IGM antibodies, which are the kind of antibodies identified by the IGM / IGG quick test, begin to rise around one week after symptoms emerge (0-7 days depending on the patient).