Vaccines have been more readily available in recent times. In most situations, an appointment is required.
A coronavirus disease 2019 (COVID-19) vaccination will help you from contracting COVID-19, as well as becoming very ill or dying from it.
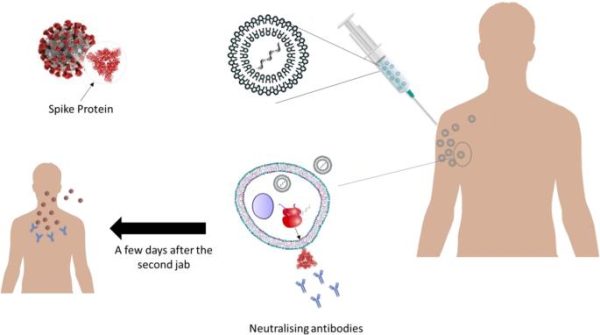
The immune system produces antibodies to combat COVID-19 after each dose of COVID-19 vaccination. COVID-19 vaccines contain a safe form of a S protein, which is a spikelike structure on the surface of the COVID-19 virus.
The highly transmissible Delta variation is driving an increase in COVID-19 infections in the United States, particularly among the unvaccinated. But the good news is that as the weeks pass, more information regarding the efficacy of currently available vaccinations and the potential of those still in research is becoming available. So, keeping up is vital, but it’s also a difficult chore, considering the deluge of information (and disinformation) bombarding us from all sides. Vaccines from Pfizer-BioNTech, Moderna, and Johnson & Johnson are now being administered in the United States, with more on the way.
In the Middle East and North Africa, a variety of COVID-19 vaccines have been authorised for general or emergency use in the last month (MENA). Understandably, there is some uncertainty about which one to select – should it, for example, be based on technology? Which one offers the most benefits? Or merely on the one chosen by a country’s government?
We’re not here to advise you which vaccination is best for you; that is, and should be, your decision. We can agree that all vaccines operate by exposing the human body to particles or molecules that stimulate an immune response, protecting the individual from illness in the future. The manner of exposure utilized differs significantly across the four main kinds of vaccinations.
What Is The Mechanism Of Vaccination?
Vaccines educate our bodies how to recognise and fight pathogens in a safe manner. They urge our immune system to create antibodies, T-cells, or both, so that our immune system knows how to fight the virus if we come across it later.
How Can We Ensure That Everyone Has Access To COVID-19 Vaccines?
To defeat the epidemic, we must defeat it everywhere on the planet. However, we will only succeed if vaccinations are available in all countries and are inexpensive. The COVID-19 Vaccine Global Access Facility (COVAX) is aiming to make this a reality by assuring that, once created, all member nations, regardless of income level, would have equal access to the vaccines in its portfolio. However, the COVAX portfolio only includes three of the vaccines now in phase III clinical studies.
Because low-income nations are less able to negotiate directly with pharmaceutical firms, there is a real risk that they may be denied vaccination access. For example, affluent nations have agreed to purchase around 600 million doses of a vaccine developed by Pfizer and BioNTech (which is not part of the COVAX portfolio). Up to the end of 2021, this accounts for roughly half of Pfizer-entire BioNTech’s manufacturing capacity. As a result, nations that have secured significant quantities of vaccine doses, such as the United Kingdom, must agree to donating any acceptable extra doses to COVAX so that they can be distributed equally as well.
Different Types of COVID Vaccines
Here is the latest list of all types of COVID vaccines that you should know about.
1. Pfizer-Biontech
After the firm announced good first clinical trial data showing the vaccine effectively avoids symptomatic illness, this became the first COVID-19 vaccine to acquire an FDA Emergency Use Authorization (EUA) on December 11, 2020. A messenger RNA (mRNA) vaccination is a relatively recent technique that employs messenger RNA (mRNA). It must be kept at freezing temperatures, making it more difficult to deliver than certain other vaccinations.
Pfizer is also the first firm to file a comprehensive approval request to the FDA for its vaccine. In addition, it says it will begin clinical trials in August to test a booster shot against the Delta strain, and it is seeking FDA approval for a third dosage, or booster dose, of its original vaccine.
2. Moderna
About a week after the Pfizer vaccination, Moderna’s vaccine was approved for emergency use in the United States. Moderna utilizes the same mRNA technology as Pfizer and has similar symptomatic illness prevention effectiveness. It should also be kept at freezing temperatures.
In February 2021, the FDA approved Johnson & Johnson’s vaccine for emergency use. Johnson & Johnson stated in November 2020 that it will start a second Phase 3 clinical research to examine if two doses, two months apart, would give greater protection. This vaccine is a carrier, or virus vector, vaccine, unlike the Pfizer and Moderna vaccines. It may be stored at room temperature in the refrigerator and is easy to distribute and administer because it only takes one injection.
3. Oxford-Astrazeneca
This vaccine, which is currently being distributed in the United Kingdom and other countries, differs from some of its competitors in terms of cost”it is less expensive to manufacture per dose, and unlike some of its competitors, it can be stored in normal refrigeration for at least six months, making it easier to distribute. The effectiveness of a booster shot is now being investigated by Oxford-AstraZeneca.
4. Novavax
Clinical studies have demonstrated that this vaccination is extremely effective. Novavax is a protein adjuvant vaccination. It’s easier to produce than some other vaccinations, and it can be kept in the fridge, making it easier to distribute. Novavax has successfully tested its vaccine in conjunction with the influenza vaccination.
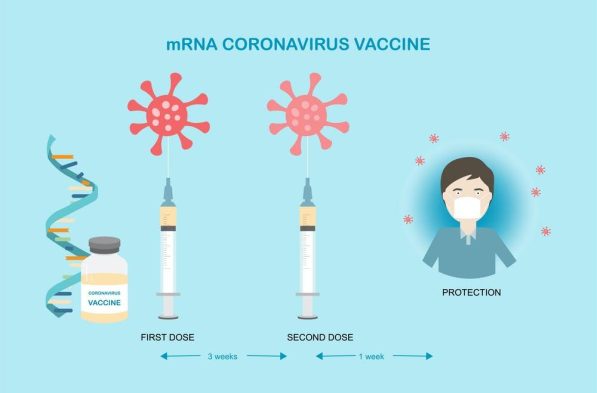
5. Messenger RNA (MRNA) Vaccine
This vaccine employs genetically modified mRNA to guide your cells on how to produce the S protein present on the COVID-19 virus’s surface. Your immune cells begin producing S protein fragments and expressing them on cell surfaces after immunisation. Antibodies are produced as a result of this. These antibodies will help you fight the COVID-19 virus if you become infected later.
The mRNA is instantly broken down after receiving instructions. It never makes it into the nucleus of your cells, which is where your DNA is stored. Pfizer-BioNTech and Moderna both employ mRNA in their COVID-19 vaccines.
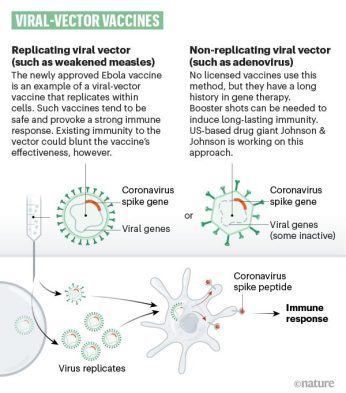
6. Vector Vaccine
The genetic material from the COVID-19 virus is put in a modified form of a different virus in this sort of vaccination (viral vector). When the viral vector enters your cells, it transmits COVID-19 virus genetic information that instructs your cells to manufacture copies of the S protein. Your immune system responds by producing antibodies and protective white blood cells when your cells exhibit the S proteins on their surfaces. If you are infected with the COVID-19 virus later, the antibodies will help you fight it.
You can’t get infected with the COVID-19 virus or the viral vector virus if you get a viral vector vaccination. Furthermore, the given genetic material does not become a part of your DNA. The COVID-19 vaccine from Janssen/Johnson & Johnson is a vector vaccine.
7. Protein Subunit Vaccine
Only the components of a virus that effectively activate your immune system are included in subunit vaccinations. This kind of COVID-19 vaccination contains S proteins, which are non-toxic. Antibodies and protective white blood cells are produced after your immune system detects the S proteins. If you are infected with the COVID-19 virus later, the antibodies will help you fight it.
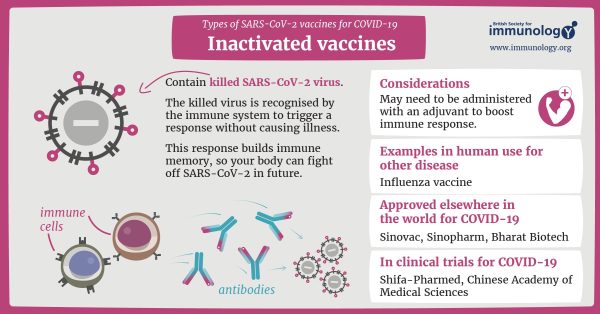
8. Inactivated Vaccine
The first step in developing a vaccine is to inactivate or destroy the disease-carrying virus or bacteria, or one that is extremely similar to it, using chemicals, heat, or radiation. This method employs technology that has been shown to function in humans ” such as the flu and polio vaccinations ” and vaccines can be produced on a reasonable scale.
However, it need specialised laboratory equipment to safely grow the virus or bacteria, can take a long time to produce, and will almost certainly require two or three doses to be delivered.
9. Live-Attenuated Vaccine
A live-attenuated vaccination employs a virus that is still alive but has been weakened or extremely similar. This type of vaccination includes the MMR (measles, mumps, and rubella) vaccine as well as the chickenpox and shingles vaccine. This method is based on the same technology as the inactivated vaccine and may be produced in large quantities. However, those with weakened immune systems may not be able to benefit from such vaccinations.
10. Protein Vaccines For COVID-19
Proteins from the SARS-CoV-2 virus are used in this vaccine, which the immune system recognizes and responds to. This reaction helps your body remember how to fight SARS-CoV-2 in the future.
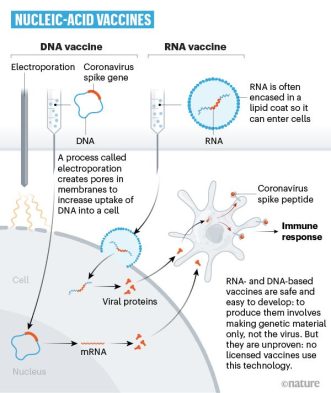
11. Nucleic Acid Vaccine
Unlike vaccines that employ a complete or sections of a weakened or dead microbe, a nucleic acid vaccine only uses a piece of genetic information that supplies the instructions for certain proteins, rather than the entire organism. Our cells employ DNA and RNA as instructions to build proteins. DNA is converted to messenger RNA in our cells, which is then utilized as a blueprint to build particular proteins.
A nucleic acid vaccine gives our cells precise instructions, either in the form of DNA or mRNA, to build the protein that we want our immune system to identify and respond to.
The nucleic acid method is a novel technique to vaccine development. None had gone through the complete regulatory procedure for use in people before the COVID-19 pandemic, however several DNA vaccines, particularly those for specific malignancies, were in human testing. Because of the pandemic, research in this field has accelerated, and certain COVID-19 mRNA vaccines have received emergency use permission, meaning they may now be given to patients outside of clinical trials.
12. Genetic Vaccines
This technique is used to educate the immune system in the Moderna and Pfizer/BioNTech COVID-19 vaccines. The vaccinations include a portion of the SARS-CoV-2 virus’s genetic material, which produces COVID-19. In the case of Moderna and Pfizer/BioNTech vaccines, the genetic material, RNA, codes for a particular viral protein. When you get a vaccination, your cells utilize the genetic material in the vaccine to produce a protein that your immune system recognizes and responds to. This reaction helps your body remember how to fight SARS-CoV-2 in the future.
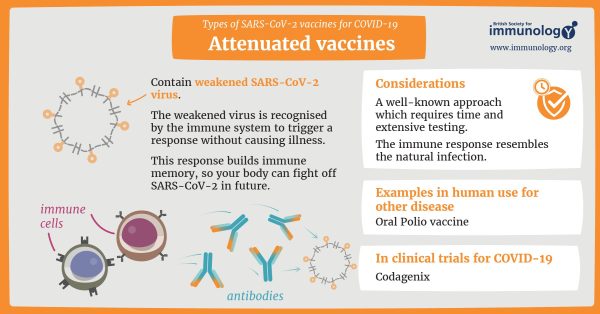
13. Attenuated Vaccines
This vaccine includes a weakened version of the SARS-CoV-2 virus, which the immune system recognizes and responds to without generating COVID-19 disease. This reaction helps your body remember how to fight SARS-CoV-2 in the future.